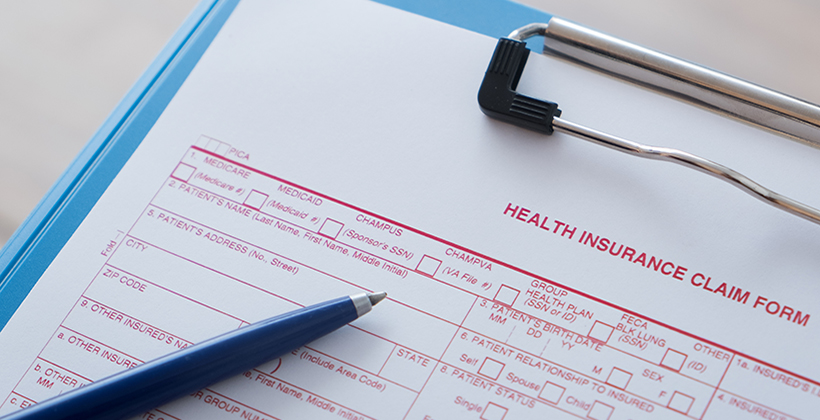
Diagnoses on a CMS-1500 Claim Form vs. Diagnosis “Pointers”
Here’s what you should know to help reduce denials
What is the difference between the diagnoses on a CMS-1500 claim form and the diagnosis “pointers” associated with each CPT® code on a CMS-1500 claim form?
A diagnosis code reflects the medical diagnosis that has been made by the provider and tells the payer why a service for which reimbursement is sought was performed. The diagnosis code must also support the medical necessity, and a failure to provide an appropriate code can be the source of a denial if the code used doesn’t support the medical necessity of the service performed.
The diagnosis “pointers” connect the medical diagnosis made by the provider to each CPT® code that is billed. When a CPT code is billed, the provider must connect or “point” the diagnosis to each procedure performed to treat the specific diagnosis, so at least one pointer per CPT code is required and the total number of diagnosis pointers per CPT code are limited to four (4). This means if a provider has more than 4 diagnosis codes for one CPT billed (i.e., procedure or treatment performed), the provider must select only four (4) diagnoses to relate to each such CPT.
In general, this means that the provider should identify the four most important or serious conditions or diagnoses that a procedure is intended to treat, which should be listed in order of severity and specifically related to the procedure code they are pointed to.
Total diagnoses and diagnosis pointers are recorded differently on the claim form. Specifically, diagnosis codes are found in box 21 A-L on the claim form and should be entered using ICD-10-CM codes. The total number of diagnoses that can be listed on a single claim are twelve (12). The diagnosis pointers are located in box 24E on the paper claim form for each CPT code billed. The line identifiers from Box 21 (A-L) should be related to the lines of service in 24E by the letter of the line.
Additional Resources
These requirements can be found in the Medicare Claims Processing Manual: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf (see pp. 14-17).
You can also find instructions in the CMS-1500 Claim Form/American National Standards Institute (ANSI) Crosswalk for Paper/Electronic Claims.
The health insurance claim form is approved by National Uniform Claim Committee (NUCC). You can find the NUCC Instruction Manual at: www.nucc.org. Approved OMB-0938-1197 FORM 1500 (02-12).