Key Telemedicine Reimbursement and Guideline Changes

Telemedicine reimbursement guidelines and other changes to billing for telehealth services you’ll want to know.
This blog was published on April 16, 2020, during the public health emergency.
In the last month, there have been a number of changes that govern using and billing for telemedicine services during the current public health crisis. Every day there seems to be a new announcement, which can make it difficult to keep up. And the federal government isn’t the only entity that’s making changes and issuing waivers to dramatically increase access to telehealth. Many states and commercial payers are also stepping up to the plate in an effort to give doctors and patients access to technology that enables continuity of care, while decreasing exposure to illness.
In this blog, we’ll highlight a few of the latest telemedicine reimbursement guidelines and other changes that you’ll want to know. What follows is intended as a general overview of these changes. Please be aware that the rules governing telemedicine and related issues are constantly changing. For up-to-date information, and additional details on the changes we describe below, please refer to the CMS’s Coronavirus Waivers & Flexibilities.
Medicare Guidelines Change: The Patient’s Home Is Now an Approved Originating Site
An originating site is defined by the Centers for Medicare and Medicaid Services (CMS) as “a location where a Medicare beneficiary gets physician or practitioner medical services through a telecommunications system.” During the current public health emergency period, Medicare has designated the patient’s home as an approved originating site. Prior to the emergency period, Medicare had generally limited traditional fee-for-service reimbursement to instances where a patient resided in a rural area, and even then, the patient still had to travel to a local medical facility to receive telehealth services from a doctor in a remote location.
Many state Medicaid programs have also waived previously existing locational requirements to permit patients to be treated from home, and many commercial payers have also taken steps to reduce their own requirements in this area.
It is also worth noting that physicians can also provide services from their homes – which also was not permitted prior to the public health emergency.
Medicare Guidelines Change: Healthcare Providers Don’t Need to Update their Medicare Enrollment to Include Their Home Location
Near the onset of the current U.S. public health emergency, providers expressed frustration that they still needed to go through the manual process of updating their Medicare enrollment to include their home location. This is no longer the case. However, the CMS recommends that providers list their home address on the patient’s claim to indicate where services were performed.
Worried that this could cause claims to be delayed or denied? The CMS had this to say: “The discrepancy between the practice location in the Medicare enrollment (clinic/group practice) and the practice location identified on the claim (provider’s home location) will not be an issue for claims payment.”
Hopefully this provides some relief to providers who don’t have time to make this update.
Medicare Guidelines Change: Billing for Telemedicine Services
Many of the billing rules and guidelines and how providers are reimbursed for telehealth have changed. Please reference the chart below for information that is consistent with the Interim Final Rule issued by the CMS on March 30, 2020, which was made effective retroactive to March 1, 2020.
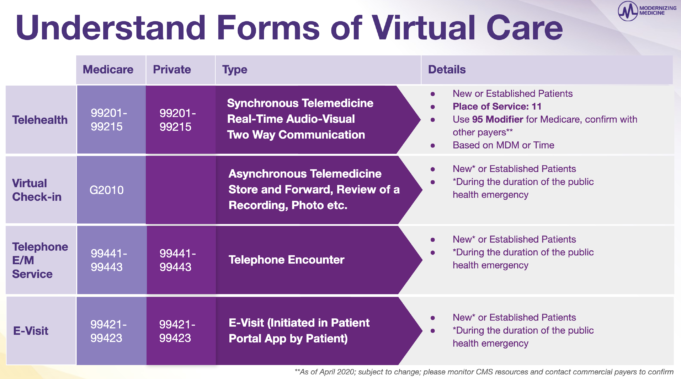
One thing to note: during the current public health emergency, providers will be reimbursed for telehealth (aka synchronous audio-video calls) as they would be for office visits. However, they must use the following codes with place of service 11 and modifier 95 when billing Medicare for services:
- Codes 99201-99205 apply to new patients
- Codes 99212-99215 apply to established patients
The CMS will apply evaluation and management (E/M) code changes similar to those that were to be effective in 2021 to all telehealth services provided during the current public health emergency, meaning that telehealth E/M levels can be selected based on medical decision making (MDM) or time (with time defined as all of the time associated with the E/M on the day of the encounter).
To reduce the potential for confusion, the CMS is maintaining the current definition of MDM. The CMS has also removed any requirements regarding documentation of history and/or physical exam in the medical record for synchronous two-way audio-visual communication telehealth visits.
Medicare Guidelines Change: More Types of Healthcare Providers Can Bill for Telehealth Services
The “who” in the “who, what, when, where and why” of telehealth (synchronous real-time audio-video) has expanded to include other types of healthcare professionals. This includes professionals like dentists and optometrists who are providing Medicare-covered services. This is good news for our clients in ophthalmology practices where optometrists often play a vital role.
Other qualified providers include:
- Physicians
- Nurse practitioners
- Physician assistants
- Certified nurse midwives
- Certified nurse anesthetists
- Certified clinical social workers
- Clinical psychologists
- Registered dietitians and nutritionists
Please review Medicare’s current billing guidance closely to ensure your practice understands what telemedicine services can be provided and billed for by non-physician providers and what supervision or similar requirements may apply.
State Law Updates: Some States Are Waiving or Reducing Licensure Requirements
Although the CMS has loosened certain requirements that would previously have prevented providers from treating patients in a state in which they were not licensed to enable health care professionals to provide and bill for telemedicine services to patients in other states, please be aware that you must still comply with all applicable state law licensure regulations. In other words, although the CMS has modified certain billing requirements to give providers a greater degree of flexibility, such modifications do not override any state law licensure regulations that might otherwise apply.
In general, most states require that a provider be licensed in the state in which the patient who they are treating is located at the time of the visit. However, many states have taken specific action to waive some of these licensing requirements during this public health emergency.
As of April 2, 2020, there is still significant variation among the approaches that have been taken by the states with regard to this issue. Some states are broadly allowing healthcare professionals who have a license in good standing in another state to provide services in their state with limited requirements, while others have adopted more limited waivers, imposing additional requirements on providers who seek to treat patients in the state without being fully licensed. Before providing services, either via telemedicine or in person, to a patient who is located in a state in which you are not licensed to practice medicine, you should consult the licensure requirements of that state, along with any updated guidance or waivers that have been issued.
Government Regulation Update: Prescribing Medications Remotely Has Gotten Easier
Both the states and the federal government regulate the prescription of medications based on telehealth consultations. However, during the current emergency, some states have loosened those requirements or have made it easier for providers to prescribe medications remotely. As was true in the case of state licensure requirements, providers should be sure to consult the laws and regulations of the state in which a patient is located before prescribing medications, particularly via telehealth.
The DEA also issued new guidelines that apply to how controlled substances are prescribed remotely via telemedicine. For the duration of the public health emergency, DEA-registered practitioners can prescribe controlled substances without first conducting an in-person medical exam as long as these conditions are met:
- The prescription must be issued for a legitimate medical purpose by a healthcare provider who’s acting within his or her scope of practice.
- The telemedicine communication that’s used must be audio-visual and real-time interactive, such as video conferencing.
- In addition to complying with the federal laws, practitioners still have to contend with the state laws that govern the remote prescription of controlled substances. Note: these laws vary state by state.
Look up your state’s laws and reimbursement policies, including those that regulate prescriptions.
HIPAA Privacy Rules for Telehealth Have Changed – At Least for Now
The Office of Civil Rights (OCR) is the agency that’s responsible for enforcing federal laws that protect privacy and security of patient information, like HIPAA. This organization has advised that it does not intend to enforce penalties under HIPAA for healthcare providers who act in good faith and use certain non-HIPAA compliant technologies, like FaceTime, to provide telemedicine services during the current public health emergency.
Please note, however, that providers would still likely be held responsible for any breaches of PHI that occur and that applicable state laws may still require that providers comply with established privacy and security requirements. Providers should exercise discretion when communicating PHI via technologies that do not comply with the HIPAA privacy and security requirements and should consider any state laws that might apply notwithstanding OCR’s current policy of non-enforcement. Where possible, providers should rely on HIPAA-compliant technology when communicating PHI or conducting telemedicine visits.
Cost-Sharing Obligations Are Getting Reduced and in Some Cases, Eliminated
Cost-sharing obligations include the co-pays, co-insurance and deductibles that commercial and government payers require providers to collect from patients consistent with each patient’s insurance policy. However, to encourage the use of telehealth, the Office of Inspector General, which typically enforces laws prohibiting providers from waiving or forgiving such patient responsible amounts, has advised that it’s not going to sanction healthcare providers who decide to waive these amounts for patients during the current public health emergency so long as the care provided is consistent with applicable Medicare coverage and payment rules, including being medically appropriate.
Many commercial payers have also decided to waive cost-sharing obligations for members who participate in covered telemedicine visits as well.
For details, please refer to your payer agreements and applicable payer policies, which are often found on the payer’s website (we’ve listed a few below, but there are many more):
Many States Have Not Eliminated or Alleviated Consent Requirements
Most states have a requirement that the provider secure the patient’s consent prior to performing a telehealth visit. Some states will dictate what needs to be in the consent form, others will control the manner in which consent is received. And unfortunately, most states have not taken steps to eliminate or alleviate telehealth consent requirements. We’ll have to wait and see if that changes.
The Stimulus Bill
This recent emergency aid package is expected to expand telehealth access and provide much-needed financial support to hospitals, community health centers and other healthcare providers.
For details, including the full text of the bill and its provisions, check out this article from USA Today.
Additional Resources
Below we’ve provided some helpful resources for providers and practices, as well a few links to specialty-specific academies and societies. This is not meant to be an exhaustive list – more of a starting point. We hope this information is helpful to you.
General Resources
- CMS Coronavirus Waivers
- Medicare Telemedicine Health Care Provider Fact Sheet
- COVID-19 State-Related Actions
- CARES Act: AMA COVID-19 pandemic telehealth fact sheet
Specialty-Specific Resources
- AAO Coronavirus and Eye Care Resources
- AAO-HNS Coronavirus Disease Resources
- AAOS COVID-19 Resource Center
- ADA Coronavirus Resources
- AGA Resources for COVID-19
- ASIPP Statement on COVID-19
- AUA Coronavirus Information Center
Modernizing Medicine has implemented its own telehealth solutions, which are available to its EMA EHR and gGastro clients.
The materials included in this blog were current as of March 26, 2020 and may be subject to change. Updates and details on the topics contained herein may be available from the CMS, the CDC, and other commercial payers. Modernizing Medicine makes no warranty regarding the ongoing accuracy of the information provided.
This blog is intended for informational purposes only and does not constitute legal or medical advice. Please consult with your legal counsel and other qualified advisors to ensure compliance with applicable laws, regulations, and standards. It is each provider’s responsibility to determine that any telemedicine visit meets medical necessity for a given patient. Not all clinical scenarios may be appropriate for telemedicine visits, and the provider may need to evaluate the patient in person to establish a diagnosis or initiate treatment.